Personal Science Week - 251218 SleepScore
Testing yet another sleep app
Three apps, three different answers. Which one is right?
This week I’m testing a new sleep app that doesn’t require a wearable. Along the way, I’ll explain why I keep tracking despite the contradictions—and why 80% of sleep improvement has nothing to do with gadgets.
The SleepScore Experiment
I’ve been trying SleepScore, the app from sleep.ai that NYTimes Wirecutter calls the best sleep app. The main selling point: no wearable required. You just point your phone’s speaker toward your bed and its “patented sonar technology”—inaudible sound waves bouncing off you— will track you throughout the night.
I tried it and it actually works! The app even comes with a test screen where you wave your hands silently in front of the phone. Cover the camera, stay quiet, and it still detects movement. Cool!
Setup quirks: My nightstand sits slightly lower than my mattress, so the first night the sonar wasn’t aimed at me and detected nothing. After repositioning, I started getting consistent results. You can try it out with the free version. For $60/year or $10/month you’ll get extras like more in-depth insights.
I’ve not been using it long enough for a rigorous review, but after a few nights of testing, the numbers don’t match my other trackers.
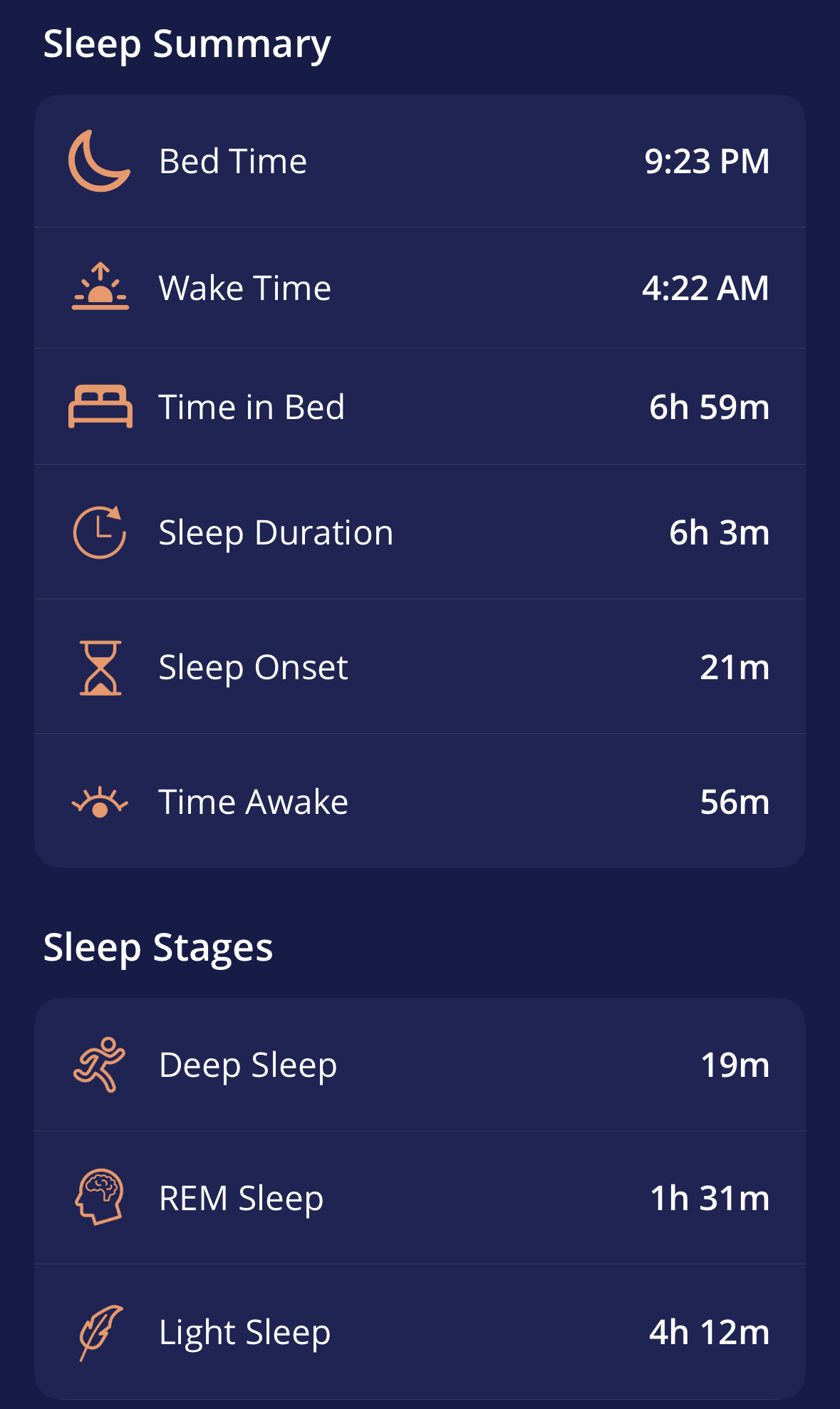
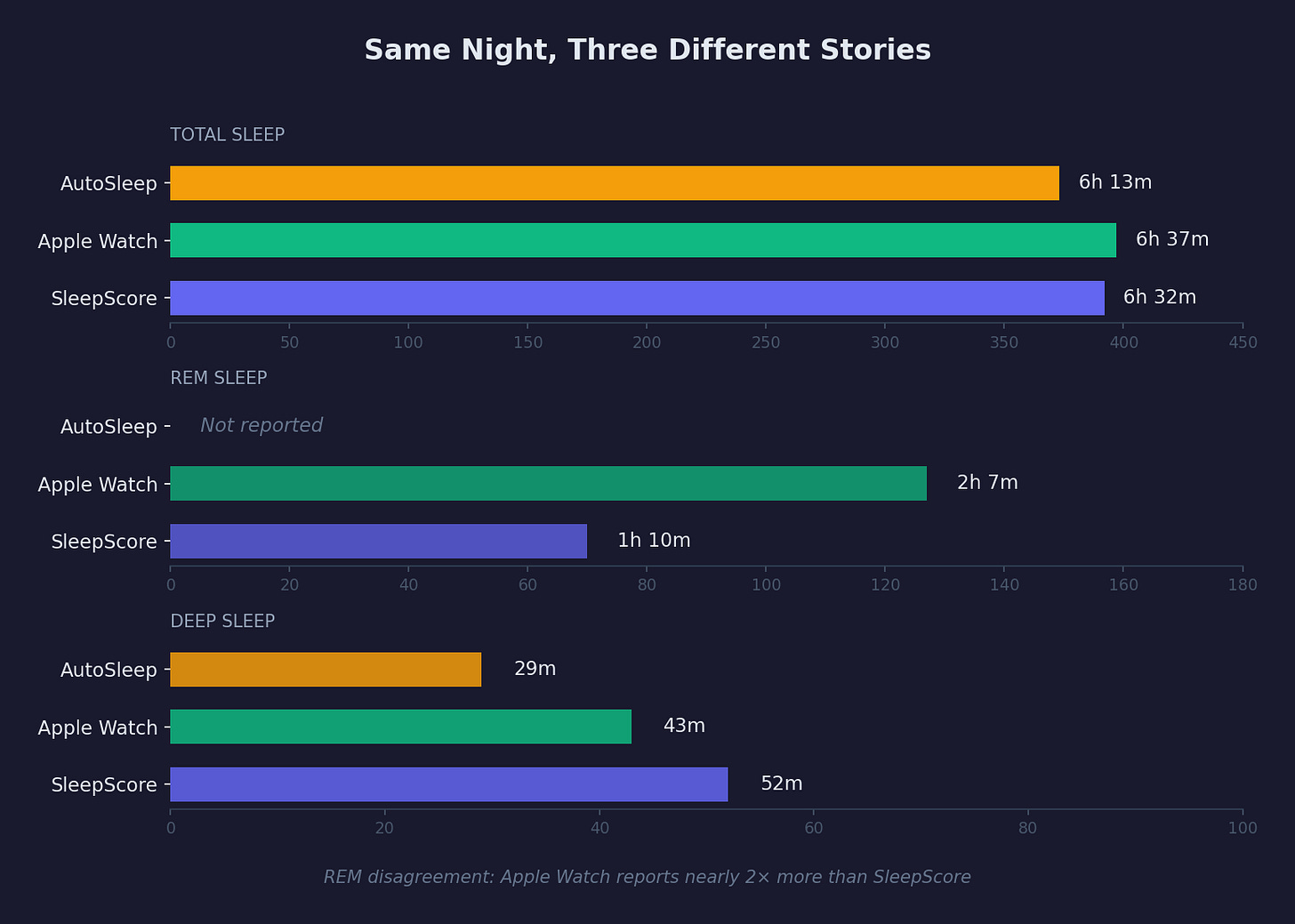
For example, here’s a typical night
Three apps. Three different stories. Which is true?
The Dirty Secret About Sleep Tracking
Here’s what years of tracking have taught me: none of them are reliably accurate, and they often don’t match how I actually feel. AutoSleep will report a “great” night when I woke up groggy; Apple Watch will show I was “awake” during periods I don’t remember at all.
This isn’t a SleepScore problem—it’s a fundamental limitation of inferring sleep stages from movement or heart rate. Even the gold-standard polysomnography (PSG) requires electrodes on your scalp measuring brain waves. Everything else is estimation.
So why keep tracking?
Two reasons:
First, long-term trends matter more than nightly scores. Any single night’s data is noisy. But patterns over months and years might reveal something real—how my sleep changes as I age, whether a new habit actually moved the needle, whether that supplement did anything (see examples below). In the decades I’ve been doing tracking, for example, I’ve learned that my long-term nightly sleep average (about 6.5 hrs) is remarkably stable.
Second, and more importantly: the tracking forces attention. This is a core insight of all my work on personal science. The “active ingredient” in most sleep improvement isn’t the gadget or the supplement—it’s the structured attention itself. When you’re tracking, you notice things. You start wondering whether that afternoon coffee mattered, whether your variable bedtime is a problem, whether alcohol is disrupting your REM.
The 80% That’s Just Obvious
I’m regularly surprised at how many people with sleep problems haven’t tried the basics. They’ll spend $300 on an Oura Ring while ignoring fundamentals that cost nothing:
Consistent bedtime (within 30 minutes, every night)
Dark room (blackout curtains, no LEDs)
Cool temperature (65-68°F)
No screens in bed
Caffeine cutoff (earlier than you think—I calculated I had ~110mg still active at bedtime from an afternoon latte)
Alcohol awareness (helps you fall asleep, wrecks your REM)
When I ran regression analysis on years of my own data using ChatGPT (see PSWeek241024), coffee was the only statistically significant predictor—reducing my sleep by over 30 minutes. Not CBD (no effect). Not most supplements. Just coffee timing. (More on caffeine genetics in PSWeek230622.)
This isn’t dismissive—it’s liberating. You don’t need expensive hardware to fix most sleep issues. You need to pay attention to the obvious stuff first.
What’s Left After the Basics
For me, after optimizing the fundamentals, one problem persists: a 3AM wakeup. I fall asleep fine, but somewhere around 3AM I’m wide awake, mind racing, and struggle to fall back asleep. This has gotten worse since 2020—now happening 5-7 nights per week.
I’ve tested various interventions:
CBD: No effect (p=0.24, later confirmed with larger dataset). See PSWeek241024.
ProdromeGlia: Actually showed statistically significant improvement in deep sleep. See PSWeek240111.
Qualia Night: No noticeable difference after 7 nights. See PSWeek241003.
I’ve also found non-pharmacological approaches helpful: the 4-7-8 breathing technique (inhale 4 sec, hold 7 sec, exhale 8 sec) to lower heart rate below 60, and remembering that quiet rest (NSDR) provides roughly equivalent benefit to actual sleep—so lying there isn’t wasted time.
Will SleepScore help with the 3AM problem? Too early to say. But I’ve signed up for their sleep study, so at least my data might contribute to something useful.
Personal Science Weekly Readings
Dr. Michael Breus has an excellent 5-minute video on what to do when you wake up at 3AM with encouraging words on why it may be less of a problem than you think.
Rob ter Horst’s YouTube channel remains the best source for rigorous sleep tracker comparisons. (tldr; get an Oura Ring)
For the genetics-curious: mutations in NPSR1 and ADRB1 are associated with people who need very little sleep (it’s not me)
I previously experimented with the SleepSpace app and its founder Dan Gartenberg in PSWeek230209
For a deep dive into using AI research tools to investigate sleep problems, see PSWeek250612 where I compared FutureHouse, Perplexity, and other LLMs on my 3AM wakeup issue
A comparison of “Deep Research” tools across multiple LLMs is in PSWeek250227
About Personal Science
Personal scientists approach sleep the same way we approach everything: with open-minded skepticism, and a willingness to experiment on ourselves. We track not because the numbers are perfect, but because tracking forces the attention that leads to insight.
We publish every Thursday. If you’ve found sleep interventions that work for you, let us know.


Really appreciate the long-term trends framing over single-night accuracy. The coffee effect being the only statistically significant predictor after regression analysis is fascinating—most people dunno their afternoon latte still has that much active caffeine at bedtime. The 3AM wakeup issue resonantes hard; glad you found the 4-7-8 breathing helps. I've had similar results with ProdromeGlia showing improvements even when CBD didn't move the needle at all. The forced attention insight is underrated too.
Let's say you can detect when you are moving, what does that tell you other than that you're not in REM sleep? I've given up on sleep tracking, beyond keeping a record of when I go to sleep and when I get up...